Ovarian Cancer
What is Ovarian Cancer?
ButtonCancer risk factors
Cancer Risk Factors
Reduce the risk
Reduce the Risk
Signs and symptoms
Signs and Symptoms
Stages of Ovarian Cancer
Cancer Statistics
What is Ovarian Cancer?
Ovarian cancer is a type of cancer that begins in the ovaries, which are the female reproductive organs responsible for producing eggs and the hormones estrogen and progesterone. It is the fifth most common cancer among women and often goes undetected until it has spread within the pelvis and abdomen.
There are different types of ovarian cancer, but the most common type is epithelial ovarian cancer, which originates in the cells that cover the outer surface of the ovary. Other types include germ cell tumors and stromal tumors, which develop from the cells that produce eggs and the connective tissue within the ovaries, respectively.
The exact cause of ovarian cancer is not well understood, but certain risk factors may increase the likelihood of developing the disease. These risk factors include a family history of ovarian or breast cancer, certain genetic mutations (such as BRCA1 and BRCA2), age, and a history of reproductive issues.
Symptoms of ovarian cancer can be vague and may include bloating, pelvic or abdominal pain, difficulty eating or feeling full quickly, and changes in bowel habits or urinary urgency. Because these symptoms can be subtle and nonspecific, ovarian cancer is often diagnosed at a later stage when it has already spread beyond the ovaries.
Risk factors for ovarian cancer include age, family history of ovarian or breast cancer, certain inherited gene mutations (such as BRCA1 and BRCA2), personal history of breast, colorectal, or endometrial cancer, and never having been pregnant. Women with a strong family history of ovarian or breast cancer may undergo genetic counseling and testing to assess their risk.
Treatment for ovarian cancer typically involves surgery to remove the tumor, and depending on the stage and characteristics of the cancer, additional treatments such as chemotherapy are usually recommended.
Early detection of ovarian cancer is challenging because there is currently no routine screening test for the general population. Women with a family history of ovarian or breast cancer or those with certain risk factors may undergo genetic counseling and testing.
It's important for women to be aware of the symptoms of ovarian cancer and seek medical attention if they experience persistent or worsening symptoms for 2 or more weeks. Regular check-ups with a healthcare provider and discussing individual risk factors can also be crucial for early detection and management.
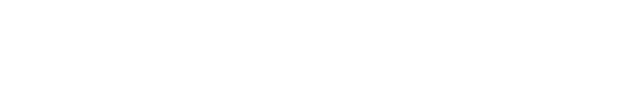
What are Ovarian Cancer risk factors?
Several factors may increase a woman's risk of developing ovarian cancer. It's important to note that having one or more risk factors does not guarantee the development of ovarian cancer, and many women diagnosed with ovarian cancer do not have identifiable risk factors. Conversely, some women with risk factors never develop the disease.
Factors that can increase your risk of ovarian cancer include:
-
Age
The risk of ovarian cancer increases as you age. It's most often diagnosed in older adults; however, ovarian cancer can and has been found at ANY age.
-
Inherited Gene Mutations
A small percentage of ovarian cancers are caused by genes changes (mutations) you inherit from your parents. The genes that increase the risk of ovarian cancer include BRCA1 and BRCA2. These genes also increase the risk of breast cancer.
Several other gene mutations are known to increase the risk of ovarian cancer, including gene changes associated with Lynch syndrome and the genes BRIP1, RAD51C and RAD51D.
-
Family history
Women with a family history of ovarian cancer, especially if it involves first-degree relatives (mother, sister, or daughter), have an increased risk. Additionally, a family history of breast, colorectal, or uterine cancer may also elevate the risk.
-
Personal history of Breast, Uterine, or Colorectal Cancer
Women who have had breast, uterine, or colorectal cancer may face a slightly higher risk of developing ovarian cancer.
-
Hormone Replacement Therapy (HRT)
Long-term use of estrogen without progesterone, often used in hormone replacement therapy during menopause, may slightly increase the risk of ovarian cancer.
-
Endometriosis
Endometriosis, a condition where tissue similar to the lining of the uterus grows outside the uterus, has been associated with an increased risk of ovarian cancer.
-
Reproductive history and infertility
Factors related to reproductive history can influence ovarian cancer risk. Women who have never been pregnant or who had their first pregnancy after the age of 35 may be at a higher risk.
- Started menstruating at an early age (before 12)
- Has not given birth to any children
- Has had first child after 30
- Experienced menopause after 50
- Has never taken oral contraceptives
- Experienced infertility: Some studies suggest that women who undergo fertility treatments may have slightly increased risk of ovarian cancer, although the overall risk remains relatively low.
It's essential to remember that while these factors are associated with an increased risk, they do not guarantee the development of ovarian cancer. Conversely, women without these risk factors can still develop the disease. Regular check-ups, awareness of symptoms, and discussing individual risk factors with healthcare providers are crucial for early detection and management.
How can you reduce the risk of Ovarian Cancer?
The following factors may decrease the risk of ovarian cancer
Diet and exercise
- A diet rich in fruits, vegetables, and whole grains may contribute to a lower risk of ovarian cancer. Antioxidants and other compounds found in these foods may have protective effects.
- Engaging in regular physical activity has been associated with a reduced risk of various types of cancer, including ovarian cancer.
Pregnancy and breastfeeding
- Women who have been pregnant and have breastfed may have a lower risk of ovarian cancer. The more full-term pregnancies a woman has had, the lower her risk may be.
5 years or more oral contraceptive use
- Oral Contraceptives (Birth Control Pills): Long-term use of oral contraceptives has been shown to reduce the risk of ovarian cancer. Women who use birth control pills for several years may experience a protective effect.
Removal of the ovaries and fallopian tubes
- For women at high risk of ovarian cancer due to genetic mutations (such as BRCA1 and BRCA2), surgical removal of the ovaries and fallopian tubes (prophylactic oophorectomy and salpingectomy) can significantly reduce the risk. This is often considered for women who have completed childbearing.
Tubal ligation
- Tubal ligation, a surgical procedure for permanent contraception (getting the "tubes tied"), has been associated with a decreased risk of ovarian cancer.
Talcum Powder
- While the evidence is not conclusive, some studies suggest a potential link between the use of talcum powder in the genital area and ovarian cancer. To reduce potential risk, some women choose to avoid talcum powder.
Consultation with a genetic counselor
- For women with a family history of ovarian or breast cancer, especially those with known genetic mutations (e.g., BRCA1 and BRCA2), genetic counseling and testing can help assess the risk. Knowledge of genetic risk factors can guide preventive measures.
It's important to note that these strategies are not foolproof, and their effectiveness can vary among individuals. Additionally, some preventive measures, such as surgical interventions, may have significant implications and should be discussed thoroughly with healthcare providers.Click here to download and share our Fact Sheet.
What are the signs and symptoms of Ovarian Cancer?
One or more of the following signs and symptoms may develop with ovarian cancer:
- Bloating
- Eating less or feeling full quickly
- Abdominal or pelvic pain (may also be back pain)
- Changes in bowel and bladder habits (constipation or diarrhea)
- Heightened fatigue
- Abnormal vaginal bleeding or discharge
Download our
fact sheet to share with others.
What are the stages of Ovarian Cancer?
Ovarian cancer is staged based on the extent to which it has spread beyond the ovaries. The staging system helps healthcare providers determine the appropriate treatment and prognosis for the disease. The most commonly used staging system for ovarian cancer is the FIGO (International Federation of Gynecology and Obstetrics) system. The stages are as follows:
-
Stage I: Cancer is confined to one or both ovaries.
- IA: Cancer is limited to one ovary, and the tumor is confined to the inside of the ovary.
- IB: Cancer involves both ovaries, with the tumor limited to the inside of the ovaries.
-
Stage II: Cancer has spread to other pelvic organs (e.g., uterus, fallopian tubes, or bladder).
- IIA: Cancer has spread to the uterus or fallopian tubes but is still within the pelvic area.
- IIB: Cancer has spread to other pelvic organs, such as the bladder or rectum, but is still within the pelvic area.
-
Stage III: Cancer has spread beyond the pelvis to the abdominal cavity.
- IIIA: Cancer has spread to the surface of the ovaries or fallopian tubes, or there are small implants on the abdominal peritoneum.
- IIIB: Cancer has spread to the peritoneum with larger implants, or there are cancerous lymph nodes in the abdominal area.
- IIIC: Cancer has spread to the peritoneum, and there are cancerous lymph nodes in the abdominal area.
-
Stage IV: Cancer has spread beyond the abdominal cavity.
- IVA: Cancer has spread to the fluid around the lungs (pleural effusion), with cancer cells identified in the fluid.
- IVB: Cancer has spread to distant organs such as the liver or lungs.
Within each stage, further sub-classification may occur based on specific factors like tumor size, the extent of spread, and involvement of nearby structures.
The stage of ovarian cancer is determined during surgery and based on a combination of factors, including the size and location of the tumor, involvement of lymph nodes, and the presence of metastasis. Staging helps guide treatment decisions, with earlier stages often having a better prognosis than later stages. It's important for individuals diagnosed with ovarian cancer to discuss their specific stage and treatment options with their healthcare team.
Ovarian Cancer statistics at a glance
| Estimated News Cases in 2023 | 19,710 |
|---|---|
| % of All New Cancer Cases | 1.0% |
| Estimated Deaths in 2023 | 13,270 |
|---|---|
| % of All Cancer Deaths | 2.2% |
5-Year Relative Survival
50.8%
2013-2019
SEER Cancer Statistics Factsheets: Ovarian Cancer. National Cancer Institute.
- The American Cancer Society estimates that in 2023, about 19,710 new cases of ovarian cancer will be diagnosed and 13,270 women will die of ovarian cancer in the United States.
- Mortality rates for ovarian cancer have declined only slightly in the forty years since the “War on Cancer” was declared. However, other cancers have shown a much greater reduction in mortality, due to many factors.
- The Surveillance, Epidemiology and End Results (SEER) Program reports that in 2019 in the United States approximately 233,565 women were alive who had been diagnosed with ovarian cancer (including those who had been cured of the disease).
- Ovarian cancer accounts for 2.5 percent of cancers in women.
- While the 11th most common cancer among women, ovarian cancer is the fifth leading cause of cancer-related death among women.
- Ovarian cancer is the deadliest of gynecologic cancers.
- Mortality rates are slightly higher for African American women than for Caucasian women.
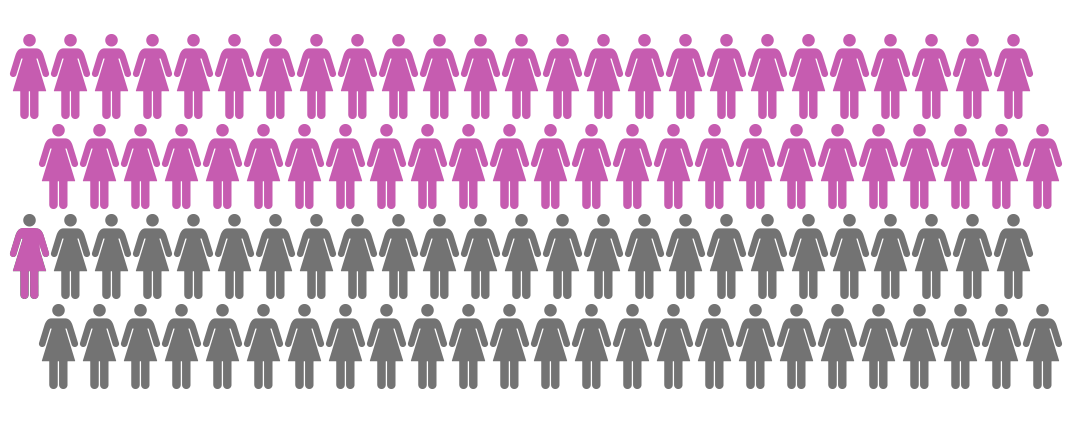
Ovarian Cancer lifetime risk and survival statistics
It’s important to be aware of the risk factors for developing ovarian cancer, as well as average rates of diagnosis. Five-year survival rates are commonly used to compare different cancers. Survival rates vary greatly depending on the stage of diagnosis.
- A woman’s lifetime risk of developing ovarian cancer is 1 in 78.
- A woman’s lifetime risk of dying from invasive ovarian cancer is 1 in 108.
- The relative five-year survival rate for ovarian cancer is 49.7% percent.
- Ovarian cancer survival rates are much lower than other cancers that affect women.
- Approximately 17 percent of ovarian cancer patients are diagnosed early with early stage disease.
- Women diagnosed at an early stage—before the cancer has spread—have a much higher five-year survival rate than those diagnosed at a later stage.
5-Year Relative Survival
50.8%
2013-2019
Ovarian Cancer statistics by age
Percentage of new cases by age group: Ovarian Cancer
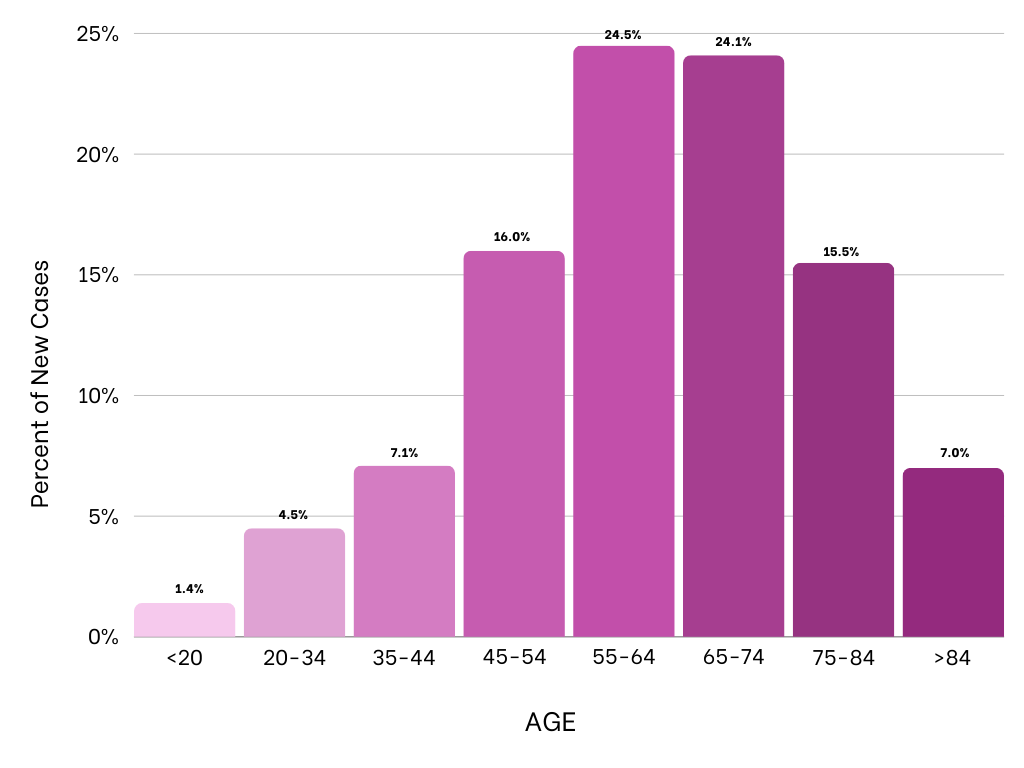
Ovarian cancer is most frequently diagnosed among women aged 55-64
MEDIAN AGE AT DIAGNOSIS
63
SEER cancer statistics factsheets: Ovary Cancer. National Cancer Institute.
- Ovarian cancer rates are highest in women aged 55-64 years.
- The median age at which women are diagnosed with ovarian cancer is 63, meaning that half of women are younger than 63 when diagnosed with ovarian cancer and half are older.
- The median age of death from ovarian cancer is 70.
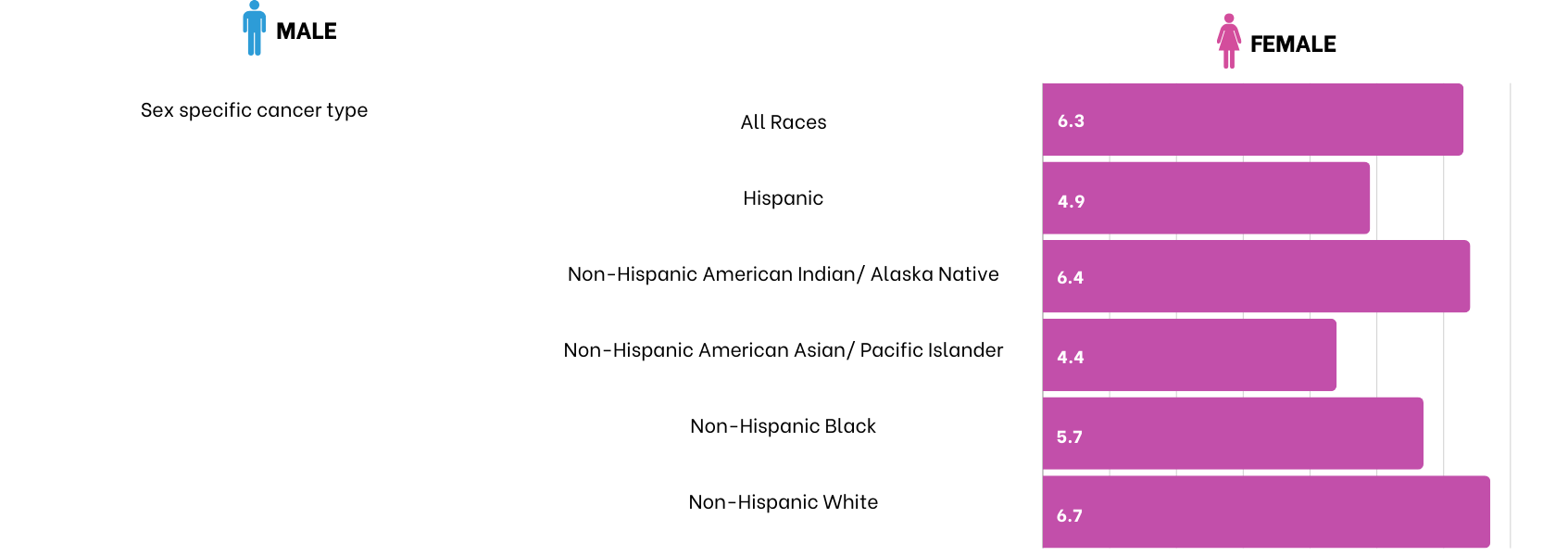
Ovarian Cancer cases by race
SEER cancer statistics factsheets: Ovary Cancer. National Cancer Institute.
For more information, visit:
Death Rate per 100,000 Persons by Race/Ethnicity: Ovarian Cancer
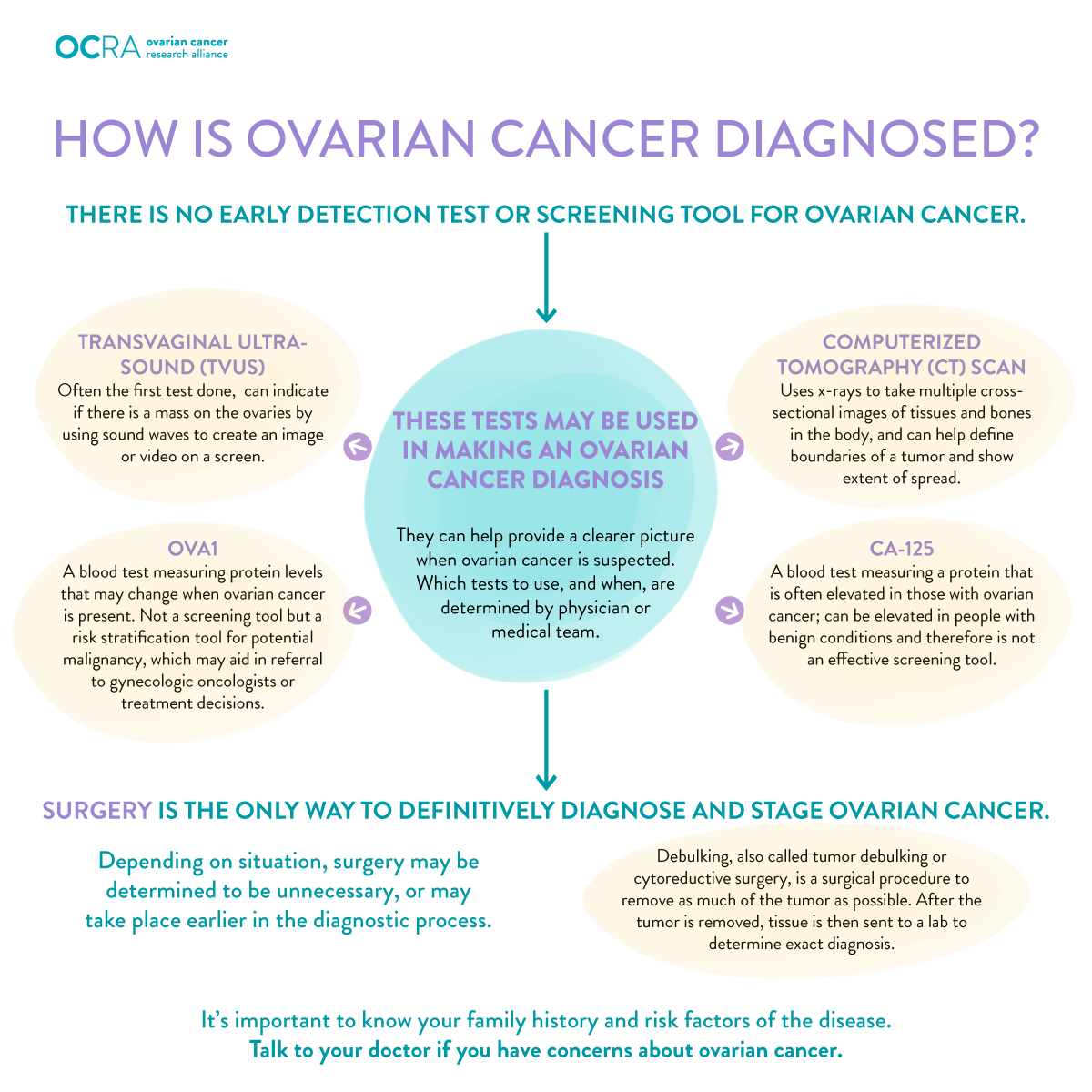
How is Ovarian Cancer diagnosed?
The diagnosis of ovarian cancer typically involves a combination of medical history assessment, physical examination, imaging studies, and laboratory tests. The process of diagnosis may include the following steps:
-
Medical history and physical examination
- The healthcare provider will take a detailed medical history, including any symptoms the individual is experiencing and any relevant family history of cancer.
- A pelvic examination may be performed to check for any abnormalities, such as ovarian masses or fluid buildup in the pelvis.
-
Imaging studies
- Ultrasound: Transvaginal ultrasound is commonly used to visualize the ovaries and detect any abnormalities. This imaging technique uses sound waves to create images of the pelvic organs.
- CT Scan or MRI: These imaging studies may be used to assess the extent of the disease and identify if cancer has spread to other areas of the abdomen or pelvis.
-
Blood tests
CA-125 Test: CA-125 is a protein that can be elevated in the blood of some women with ovarian cancer. While this test can be useful, it is not specific to ovarian cancer and may be elevated in other conditions, such as endometriosis or pelvic inflammatory disease.
-
Biopsy
A definitive diagnosis of ovarian cancer is usually confirmed through a biopsy, where a sample of tissue is taken for examination under a microscope. This can be done through surgery or a less invasive procedure called a laparoscopy.
-
Surgical exploration
(Exploratory Laparotomy or Laparoscopy)
In many cases, surgery is performed to explore the abdominal and pelvic cavity, obtain tissue samples for biopsy, and determine the extent of the disease. This may involve removing one or both ovaries, fallopian tubes, and the uterus.
-
Staging
The extent of the cancer is determined through surgical staging, which involves examining tissues and organs within the pelvis and abdomen to determine the stage of the cancer.
It's important to note that the diagnosis and staging of ovarian cancer involve a multidisciplinary approach, with input from gynecologic oncologists, radiologists, pathologists, and other healthcare professionals. Early detection of ovarian cancer can be challenging because symptoms are often vague and nonspecific. Due to the lack of routine screening tests for the general population, awareness of symptoms and prompt medical attention are crucial. Women who experience persistent or worsening symptoms, such as abdominal bloating, pelvic pain, or changes in bowel habits, should seek medical evaluation.
Who treats Ovarian Cancer?
Gynecologic oncologists are crucial for ovarian cancer patients due to their specialized training and expertise in the management of gynecologic cancers, including ovarian cancer. Here are several reasons why gynecologic oncologists are considered imperative for the care of ovarian cancer patients:
Specialized training
Gynecologic oncologists undergo extensive training specifically focused on the diagnosis and treatment of gynecologic cancers. This includes ovarian cancer, as well as cancers of the uterus, cervix, vulva, and other reproductive organs.
Surgical expertise
Gynecologic oncologists are skilled surgeons who specialize in the surgical management of gynecologic cancers. Surgical intervention is often a key component of ovarian cancer treatment, involving procedures such as hysterectomy, removal of ovaries and fallopian tubes, and debulking surgery to remove visible tumors.
Optimal surgical staging
Accurate staging of ovarian cancer is essential for treatment planning. Gynecologic oncologists are trained to perform comprehensive surgical staging, which involves assessing the extent of the disease and determining the appropriate treatment approach based on the stage.
Chemotherapy administration
Gynecologic oncologists are experienced in the administration of chemotherapy, a common treatment for ovarian cancer. They develop and oversee chemotherapy regimens tailored to the specific characteristics of the cancer, considering factors such as the type and stage of the disease.
Clinical trials and research
Gynecologic oncologists often have access to and participate in clinical trials, which are research studies evaluating new treatments or approaches for ovarian cancer. Involvement in clinical trials allows patients to access cutting-edge treatments that may not be available elsewhere.
Multidisciplinary care coordination
Gynecologic oncologists work collaboratively with other specialists, such as medical oncologists, radiation oncologists, radiologists, and pathologists, to ensure comprehensive and coordinated care for ovarian cancer patients. This multidisciplinary approach optimizes treatment outcomes.
Expertise in fertility-sparing options
For women of childbearing age who wish to preserve fertility, gynecologic oncologists can discuss and implement fertility-sparing options whenever possible while ensuring effective cancer treatment.
Genetic counseling and testing
Gynecologic oncologists often work with genetic counselors to assess the risk of hereditary ovarian cancer and offer genetic testing to identify relevant mutations, such as BRCA1 and BRCA2.
Comprehensive follow-up care
Gynecologic oncologists provide ongoing monitoring and follow-up care for ovarian cancer survivors, addressing potential side effects of treatment, managing recurrence, and promoting overall well-being.
Given the complexity of ovarian cancer and the importance of specialized care, gynecologic oncologists play a central role in guiding patients through the diagnosis, treatment, and survivorship phases of ovarian cancer. Patients diagnosed with ovarian cancer are often encouraged to seek consultation with a gynecologic oncologist early in the management process to benefit from their expertise and experience.
How to find a Gynecologic Oncologist in your area:
- Visit the Foundation for Women’s Cancer website to search for a gynecologic oncologist near you
- Ask your primary care doctor or gynecologist for a referral
- Call the nearest hospital or community-based cancer center
- Get a second opinion if needed: Even doctors sometimes feel they need to get a second opinion on the results of the pathology report after surgery. You should feel you have the right to get a second opinion, if you want one.
Clinical trials
Find clinical trial options here:
Additional help in selecting your next cancer treatment
Travera
Ovarian cancer is a particularly challenging disease that often goes undetected until it reaches an advanced stage. For those grappling with ovarian cancer, standard treatments like surgery, chemotherapy, and targeted therapy may have limited effectiveness.
However, alternative therapeutic options can enhance patients' quality of life, extend survival, and instill hope: ex-vivo cancer drug testing is an increasingly practical approach for individuals seeking insight on effective ovarian cancer treatments.
Through a special partnership with Colleen’s Dream Foundation and Travera, you may be able to receive this newly available test at NO COST.

Watch this video to learn how Travera’s First in Class Ex-Vivo Cancer Drug Testing can evaluate a broad range of FDA-approved drug options to assess their potential for treating your unique cancer.
To find out if you may qualify for this NO COST testing, learn more about how to best share this with your doctor, or just get more of your questions answered, please contact Dennis Watson with Travera at dwatson@travera.com or call
781-874-0808
Frequently asked questions
CONTACT:
Media Inquiries:
Disclaimer: Colleen’s Dream Foundation, Inc. (“Colleen’s Dream”), is an Arizona nonprofit corporation recognized by the IRS as a tax-exempt public charity under Section 501(c)(3) of the Internal Revenue Code (Federal Tax ID: 45-5323829), which operates through a fiscal sponsorship with Players Philanthropy Fund, a Texas nonprofit corporation recognized by IRS as a tax-exempt public charity under Section 501(c)(3) of the Internal Revenue Code (Federal Tax ID: 27-6601178). All contributions to Colleen’s Dream qualify as tax-deductible to the fullest extent of the law.
All Rights Reserved | Colleen’s Dream Foundation
All Rights Reserved | Colleen’s Dream Foundation